News
NEW Online Request Proforma - AccuRX
We have changed our online request provider from eConsult to AccuRX. It is live from today (1st December).
We believe this will be easier to complete, as it asks fewer questions, and does not try to collect information such as smoking status, alcohol consumption, weight, etc.
Your requests will be responded to by 7pm on the day of submission.
You can find the link on our website home page below the welcome message, along with a link to a you tube video that shows you how to use AccuRX.
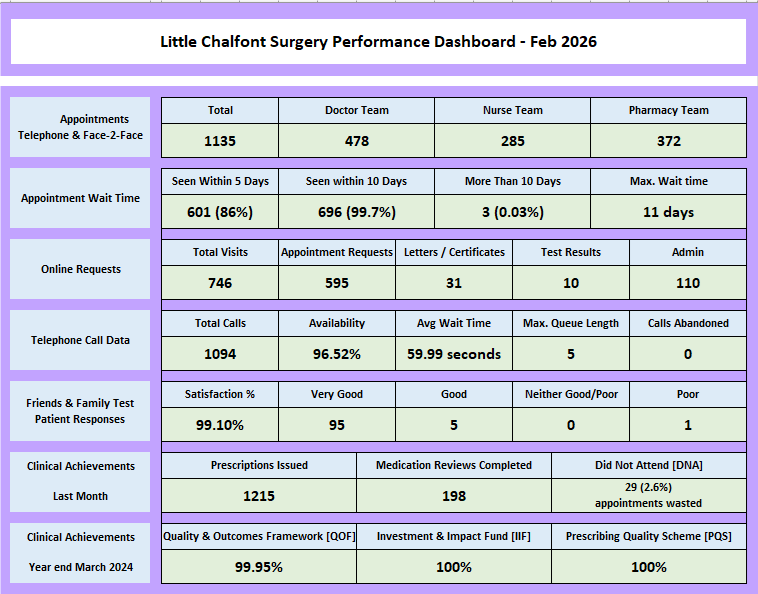
Sharing Our Performance...
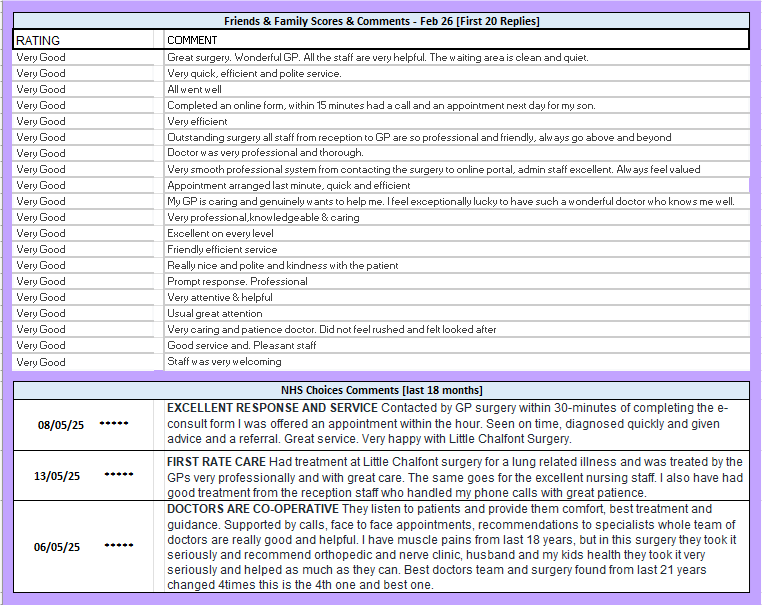
Sharing Our Feedback...
School Age Children Requiring Flu Vaccination
In response to the news stories of a nationwide rise in flu cases the Buckinghamshire School Aged Immunisation Team (SAI) have been receiving a significant number of telephone calls from parents regarding flu vaccinations. These include parents who have previously declined the offer or parents of children who may not have been at school on the day the SAI team visited and whose children remain unvaccinated.
If you are seeking a flu vaccination for a school-aged child, please contact Buckinghamshire SAI, who will be providing additional clinics.
They can be contacted via telephone on 01494 323000 or email at buc-tr.BucksChildImms@nhs.net.
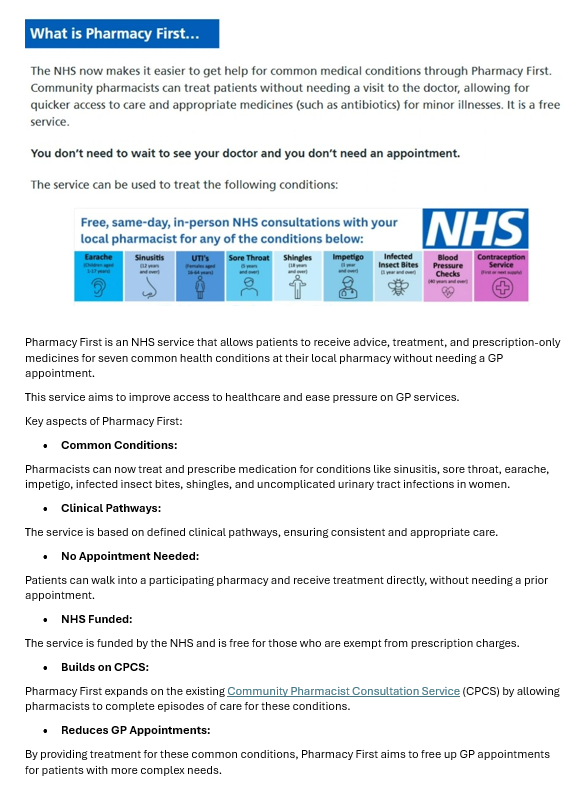
Pharmacy First
Jess’s Rule: Three strikes and we rethink
What is Jess’s Rule?
Jess’s Rule asks GP teams to ‘reflect, review and rethink’ if a patient presents three times with the same or escalating symptoms.
Reflect: Think back on what the patient has said and consider what has changed or been missed. Offer ongoing episodic continuity of care for future direct patient care. If previous consultations have been remote, see the patient face-to-face and conduct a physical examination.
Review: Where underlying uncertainty exists, consider seeking a view from a peer and review any red flags that may suggest another diagnosis, regardless of the patient’s age or demographic.
Rethink: If appropriate, refer onwards for further tests or for specialist input.
How Jess’s Rule will benefit patients
Under Jess’s Rule, listening carefully to the patient’s concerns and taking note of each symptom remain crucial, recognising that patients are experts about what feels normal for their body. Joint decision-making between the clinician and patient remains key in this process.
It is asking for GP teams to rethink the accuracy of their diagnosis, really listening to the patient and taking note of each symptom or concern. This may mean seeing a patient face-to-face and conducting a physical examination if previous consultations have been remote.
After consulting again with the patient, Jess’s Rule encourages GP teams to re-evaluate why the patient’s condition remains unresolved by an existing treatment plan and/or consider why their symptoms are escalating.
Jess’s Rule encourages consistency of care but prompts GP teams to consult with one another to jointly reconsider any red flags that have been missed that could point to another diagnosis, and to challenge any assumptions that may have been made based on a patient’s age or demographic.
Here at Little Chalfont Surgery we offer continuity of care for this very reason, and hold clinical education meetings every Monday - complex problems, or diagnosis which are not clear are discussed within the clinical team to benefit from the vast experience amongst the clinicians, this usually identifies a productive way forward which in certain instances would include an onward referal for a more detailed or specialist assessment.
Food Support Schemes in Buckinghamshire
Many people are struggling with the cost of living. The Government has some suggestions and resources to help and support.
https://www.gov.uk/cost-of-living/managing-money
With the cost of living soaring, more and more people are struggling to feed themselves and their families.
There’s nothing worse than hunger when you’re cold, and if you’re struggling to feed yourself or your children, a food bank can supply an emergency parcel with enough food for at least three days.
To receive support from a food bank, you’ll need a referral for a food voucher. Contact your local Citizens Advice: https://www.citizensadvice.org.uk/debt-and-money/food-bank/using-a-food-bank/
If you don’t have enough food and cannot afford to buy food, you may be able to seek support from the Trussell Trust. If you’re really struggling to feed yourself or your family, foodbanks could help you manage for a few days. They can also help and signpost you to other support.
The Trussell Trust is a national foodbank organisation. Visit: https://www.trussell.org.uk/
Remember, if you are in need, your local foodbank is there to help:
https://www.trussell.org.uk/emergency-food/find-a-foodbank
There are also independent foodbanks. Buckinghamshire Council website has information and support: https://familyinfo.buckinghamshire.gov.uk/advice-and-support/money-and-benefits/help-with-essentials/
FOODBANKS – serving those in need
- Chiltern Foodbank, 71 The Broadway, High St, Chesham HP5 1BX
Tuesday – Friday 10:30 – 12:30 (voucher based) - (Chesham) FoodLife – Restore Hope, The Estate Office, Latimer Park, Latimer, Chesham, HP5 1TU https://www.restorehopelatimer.org/foodlife/ (families only)
- High Wycombe/ South Bucks – One Can Trust, 11B Duke Street, High Wycombe, HP13 6EB
referral based
COMMUNITY FRIDGES – helping food go the extra mile – all welcome
- Chesham – next to the Broadway Baptist Church, Chesham, HP6 1EG
Wednesday 10:00 – 12:00am, Saturday 10:00 – 12:00am. - High Wycombe – Oakridge Baptist Church, High Wycombe, HP11 2PH
Monday 9:30am – 2:30pm, Wednesday 9:30am – 2:30pm - Chalfont St Giles – All Together Community Fridge, Blizard’s Yard Car Park, High Street, HP8 4QA
Wednesdays 10:00 – 12:00 and Saturdays 10:00 – 12:00
FOOD HUBS – no one in our community should have to face going hungry
- Wycombe Food Hub, Chilterns Shopping Centre, High Wycombe, HP13 5ES
Monday, Tuesday, Thursday, Friday & Saturday 11am – 2pm
Additional Support
High Wycombe Central Aid: Help local people who are in need and/or on a low income with basic essential furniture and electricals.
For those in need of a little extra support to access food, there are lots of wonderful agencies and schemes running within Buckinghamshire.
Buckinghamshire Council have several schemes available to residents in Buckinghamshire, including grants, insulation programs and support and guidance, for more information visit: Buckinghamshire Council Keep Warm
Cost of Living Information and Support
Buckinghamshire Council has published a number of avenues that may support our patients, including access to free or low cost food, financial support and help with other living costs.
Click the link for more information: https://www.buckinghamshire.gov.uk/cost-of-living/?utm_medium=email&utm_name=&utm_source=govdelivery
Winter weather warnings and staying warm
Feeling the chill this winter? Keeping warm is essential for your well-being and health. Winter weather can stop vulnerable people getting out and about, so it’s important to check on your neighbours and friends during this time.
When it’s cold outside, and inside, there are some tips you can use to preserve heat and keep warmer:
Reduce draughts where you can
- Layer up – wear lots of layers of thinner clothing
- Cover extremities – hats, gloves, thick socks and scarves
- Eat healthily with plenty of hot drinks
- Avoid alcohol
- Keep moving
- Hot-water bottles are a great, cost-effective way to keep warm
- Look into financial support such as the winter fuel payment
Keeping the cold at bay can help you stay healthy over the wintry months. https://www.ageuk.org.uk/informatio...keep-well-this-winter/stay-healthy-in-winter/
https://www.gov.uk/winter-fuel-payment
Digital Portal for patient communication in to the practice - AccuRX
As part of the NHS Digital Transformation plan, all practices are required to have a digital platform.
Our digital platform or online service is called AccuRX and is available through the week.
It can be accessed via our website, from your mobile, tablet or PC, or the NHS App. There is no need to download an app.
AccuRX is a service for patients wanting to contact the GP to request routine appointments, medication requests along with any queries, either clinical or administrative. You should receive a response for medical matters on the same day, and for admin matters within two working days.
Avoid calling the practice where possible as our phone lines are very busy.
Simply use AccuRX, the link button is located on our home page, and avoid the queues.
FOR PATIENTS WITH CLINICALLY URGENT PROBLEMS NEEDING AN ON-THE-DAY APPOINTMENT, PLEASE CONTINUE TO PHONE AT 08:30 OR AS SOON AS POSSIBLE.
How We Are Operating 'Post Covid'
We are now 'living with Covid'. Since April 23 the wearing of PPE and patients required to wear masks has been stood down.
However, if you or a member of your household has 'Covid' or chest infection symptoms we do request that patients wear masks when vising the surgery.
This is in place to:
1. lower the risk of Covid virus transmission from patients to staff and vice versa.
2. reduce the viral load of Covid in the building, which is essential to ensure we can protect the patients attending the surgery daily for face-to-face appointments, which include vulnerable patients and very young babies receiving their immunisations. As well as protect the surgery team from over exposure to high levels of the Covid virus, which in turn ensures the surgery remains open and able to offer a GP Service to the residents of Little Chalfont.
In line with the NHS 10 year Digital Transformation Plan, we opeate a digital total triage service; our chosen software system is called AccURX, this allows patients to contact the surgery requesting advice, self-help, medication, admin requests, etc. Many of our patients had been asking for a way to contact the surgery without waiting on the phone, and this provided the answer.
Using AccuRX you can contact us from work, home, or while commuting, without having to wait to get through on the phone. The information you provide is delivered to a secure inbox to your GP, who then determines next steps, this could be asking for more information, providing a medicine or treatment plan, or arranging a consultation – either telephone, video or face-to-face. We aim to respond to you by the end of the next working day.
To access this go to our website home page and click on the large banner - AccuRX.
To access the surgery - Select the relevant section, and follow the prompts to provide the requested information. This is powered by Artificial Intelligence (AI) so your next question is determined by your previous answer.
For advice and guidance, scroll down the page and select from
- Condition
- A-Z
- For your Child
- Body Map
You can then decide whether you want self-help; pharmacy advice; or advice and treatment from your GP
Reception is open to assist patients with queries Monday to Friday from 10:30 - 12:30 and 15:00 to 17:00.
HELP US TO HELP YOU
Please review our website which is updated very regularly, it contains lots of information for services that are available to help and support you, many of these you can access directly without a referral from your GP.
Only contact us when your GP Surgery Team are appropriate people.
For minor ailments, self-treat or speak to a pharmacist for advice; they will know when it is appropriate for you to contact your GP. All pharmacies in buckinghamshire now offer a Pharmacy First service, which includes issuing medication for some conditions and illnesses. for more information about the Pharmacy First scheme, visit - https://www.england.nhs.uk/primary-care/pharmacy/pharmacy-services/pharmacy-first/
For minor injuries, there is a GP-led Urgent Treatment Centre at Wycombe General Hospital, open 8am to 8pm every day, to obtain an appointment for this phone 111.
The UTC Treats:
- cuts and bruises
- sprains and strains
- bites and stings
- scalds and minor burns (but not involving the head or neck),
- infected wounds
- suspected fractures
- minor head injuries (no loss of consciousness) – ADULTS ONLY*
- objects lodged in ear/eye/mouth/nose
*Children should attend A&E at Stoke Mandeville
If you are unsure, always call NHS 111, who also provide a 24/7 advice service.
Information from The Infected Blood Enquiry
The Infected Blood enquiry focused on patients who received blood transfusions and blood products between 1970 and 1996, and is now complete.
The final report was published on 20 May 2024. Visit: https://www.infectedbloodinquiry.org.uk/reports
Although it is likely that the majority of those who were directly affected have now been identified and started on appropriate treatment given the time that has elapsed since the last use of infected products, there may be people who have not yet been identified, particularly if they are living with asymptomatic Hepatitis C.
Some patients will already have been contacted by the blood service as part of the ‘lookback investigations’ which began in the mid-1990s following introduction of HIV and Hepatitis C screening.
What to do if you think you may have received blood in the 1970s and 1980s
If you received blood or blood products prior to 1992, and were not contacted but think you might be at risk of Hepatitis C, please visit: https://hepctest.nhs.uk/. This NHS website enables patients to request a simple finger prick blood test kit to do at home and post back to the lab, results received within 2 weeks.
It is very unlikely that anyone who has HIV following blood transfusions in the 1970s and 1980s is not already diagnosed and aware of their infection.
For those who are concerned about the risk of HIV infection, further information can be found here: https://www.nhs.uk/conditions/hiv-and-aids/diagnosis/ and here: https://www.nhs.uk/service-search/other-health-services/hiv-testing
Hepatitis B, another infection that can be linked to infected blood, usually clears up on its own without treatment; however, if you are concerned about Hepatitis B infection more information can be found here: https://www.nhsbsa.nhs.uk/england-infected-blood-support-scheme or your local sexual health clinic: https://www.nhs.uk/service-search/sexual-health/find-a-sexual-health-clinic
The government has published guidance for patients, please visit: https://assets.publishing.service.gov.uk/media/5d1613ec40f0b609da30d37c/Information_for_patients_on_the_Infected_Blood_Inquiry.pdf
Patients and families affected/infected are entitled to compensation. More information about the compensation scheme can be found here: https://www.gov.uk/government/publications/infected-blood-compensation-scheme-summary/infected-blood-compensation-scheme-summary
Buckinghamshire, Oxfordshire and Berkshire West Integrated Care Board [BOB ICB]
As part of a government change to the structure of the NHS, Buckinghamshire, Oxfordshire and Berkshire West Clinical Commissioning Groups [CCGs] merged to become BOB ICB.
They have launched a stakeholder newsletter to enable patients to keep abreast of the current services and changes being proposed in hospital and community care.
To view the nesletter, please visit: https://content.govdelivery.com/accounts/UKBOBICS/bulletins/3a14197
If you wish to subscribe to the newsletter, clicl on the link above, scroll to the bottom of the home page and subscribe. You can unsubscribe at any time.
Page created: 13 October 2020